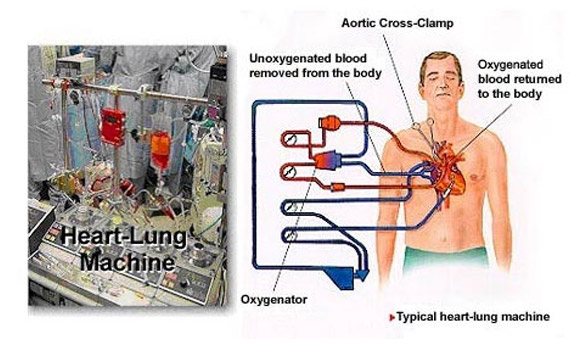
Open heart surgery is any surgery where the chest is opened and surgery is performed on the heart muscle, valves, arteries or other heart structures, such as the aorta. These are called ‘open heart surgeries’ because, while the surgery on the heart is being done, the heart lung machine is used.
The heart lung machine is a medical equipment that temporarily takes over the function of the heart and the lungs during the surgery, maintaining the circulation of the blood and the oxygen content of the body, and thus helps to provide oxygen rich blood to the brain and other vital organs, and the technique used is called ‘cardio pulmonary bypass’ (CPB). Cardiopulmonary bypass is commonly used in heart surgery because of the difficulty of operating on the beating heart. The heart is made still or motionless with the help of medications. It also provides a relatively blood free operating area.
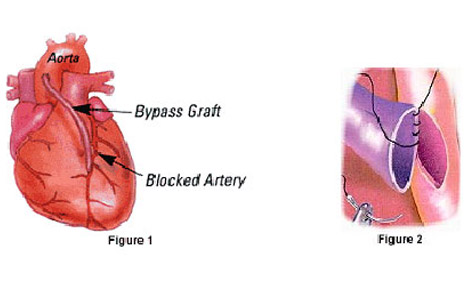
CABG is an acronym for Coronary Artery Bypass Graft. Just like any other organ or structure of the human body to function and survive, the heart also needs nutrients and oxygen rich blood supply. This is provided by the coronary arteries which are the blood vessels of the heart muscle, the myocardium. These relatively narrow vessels are commonly affected by atherosclerosis and become blocked or clogged, causing chest pain (angina) or a heart attack (myocardial infarction). CABG (pronounced ‘cabbage’) surgery, also called Coronary Artery Bypass surgery, and colloquially ‘heart bypass’ or ‘bypass surgery’, is a surgical procedure, wherein alternate channels or routes are created to provide nutrients and oxygen rich blood supply to the heart muscle beyond the blockages in the coronary arteries, and thus relieve angina and prevent myocardial infarction.
CABG surgery is recommended for patients with angina in whom the medical treatment has failed and they are not suitable candidates for angioplasty (stenting). It is the ideal procedure for patients having multiple blocks in multiple coronary arteries and their branches. Long term results of CABG are better in patients having severe (critical) block in the left main coronary artery, in patients having multiple blocks (triple vessel disease) with poor pumping (ejection fraction) of the heart and diabetics. It is also done in emergency situations in patients who become very critical during angioplasty and stenting.
It is not appropriate or feasible in all patients. Patients with non critical disease can be managed medically and certain patients with single or double vessel disease are better candidates for angioplasty and stenting. Patients with diffuse coronary atheroma with poor target arteries and those with occluded coronary vessels without lumen, are not suitable for CABG. In some patients with significant co- morbid conditions CABG may be prohibitive.
The bypass is created using either an artery from inside the chest (internal mammary artery), an artery from the forearm (radial artery) or vein from legs or a combination of three. The patency of arterial graft is longer and it prolongs the benefit and survival of the patient. Hence it is preferable to use more of arterial conduits especially in young patients (Total Arterial Revascularization).
The conventional and most widely preferred approach to perform any cardiac operation world over is carried out by opening (sawing) the entire length of the breast bone (sternum) after making an incision down the middle of the chest. This procedure is called a median sternotomy (cutting of the sternum). Bypass grafts (vessels or ‘conduits’) have to be taken (harvested) to do the bypass operation The most commonly used vessel for the bypass is the left internal mammary artery and saphenous vein from the leg. Bypass grafting involves sewing the graft vessels to the coronary arteries beyond the narrowing or blockage. The other end of this vein is attached to the aorta. Chest wall arteries, particularly the left internal mammary artery, have been increasingly used as bypass grafts. This artery is separated from the chest wall and usually connected to the left anterior descending artery and/or one of its major branches beyond the blockage. Before bypass surgery can take place, a cardiopulmonary bypass must be established. Plastic tubes are placed in the right atrium to channel venous blood out of the body for passage through a plastic sheeting (membrane oxygenator) in the heart lung machine. The oxygenated blood is then returned to the body. The main aorta is clamped off (cross clamped) during CABG surgery to maintain a bloodless field and to allow bypasses to be connected to the aorta. CABG surgery takes about four to six hours to complete. The aorta is clamped off for about 60 minutes and the body is supported by cardiopulmonary bypass for about 90 minutes. The use of 3 (triple), 4 (quadruple), or 5 (quintuple) bypasses are now routine. At the end of surgery, the sternum is wired together with stainless steel and the chest incision is sewn closed. Plastic tubes (chest tubes) are left in place to allow drainage of any remaining blood from the space around the heart (mediastinum). About 2% of patients require exploration within the first 24 hours because of continued bleeding after surgery. Chest tubes are usually removed two days after surgery. The breathing tube is usually removed a few hours after surgery. Patients usually get out of bed and are transferred out of intensive care two days after surgery. A new advance for many patients is the ability to do CABG with out going on cardiopulmonary bypass (“off pump”), with the heart still beating, also, popularly known as ‘beating heart’ CABG.
In the past decade many cardiac surgeons have adopted and adapted to the technique of “off-pump” CABGs, so much so that, in my practice, now over 98% of the CABG surgeries are “beating heart” procedures, which is also known as Off Pump Coronary Artery Bypass (OPCAB). Off pump beating heart surgery allows patients to forego cardiopulmonary support and the operations are conducted on protected, motionless hearts, wherein the precise area of operation is kept still with the use of stabilizing devices. This technique offers the patients faster post-operative recovery, less adverse effects on their systems, shorter hospital stay, overall mortality less than 1%, and an early return to a productive life.
Minimally invasive coronary artery surgery is also called limited access coronary artery surgery (MICAS). MICAS is performed by accessing the heart through the left chest with a small 6 cm incision. MICAS is used to avoid the heart-lung machine. It’s done while the heart is still beating and is intended for use when only one or two arteries will be bypassed. MICAS uses a combination of small holes or “ports” in the chest and a small incision made directly over the coronary artery to be bypassed. Usually an artery from inside the chest wall is detached and re-attached to the clogged coronary artery farthest from the occlusion. The attachment is performed directly under vision, so the artery to be bypassed must be right under the incision.
There is an alternate minimally invasive approach called the LESS (Lower End Sternal Split) procedure that can be offered to the patient to undergo bypass operation. In this procedure only the lower half of the sternum (breast bone) is split to access the heart.
MICAS procedures provide not only a better cosmetic result but also better long term results with quicker recovery to active lifestyle.
If you’re a candidate for CABG, the benefits of having the surgery include: Significantly improves your quality of life and decreasing angina and other symptoms, Improves exercise capacity allowing you to resume a more active lifestyle, Improves the pumping action of your heart if it has been damaged by a heart attack, Lowers the risk of a heart attack . Significantly improves your chance of long term survival. Those with the most severe Coronary Artery Disease gain maximum from CABG operation.
Coronary Artery Bypass Grafting is a safe operation with overall elective surgical mortality related to CABG of around 1% in good LV function. During and shortly after CABG surgery, heart attacks can occur in 1% of patients and are the main cause of morbidity. About 2% of patients require exploration because of bleeding. Stroke occurs in 1-2%, primarily in elderly patients. The risk of stroke is reduced, but not eliminated completely, by beating heart surgery. Various factors influence surgical mortality including age, sex, degree of cardiac dysfunction and other co-morbid conditions including obesity, renal impairment, carotid artery disease etc.
For CABG early failure rate is about 5% (some venous grafts may be blocked). Thereafter about 2% a year upto 10 yrs. Majority of the patients enjoy better long-term benefits after CABG rather than Angioplasty. The commonest cause of graft blockage is development of atheromatous disease in the grafts. Aggressive lifestyle modification and control of serum lipids prolongs graft patency. In people who are candidates for the surgery, the results usually are excellent. Following CABG, 90 percent of people have significantly reduced symptoms, less risk of future heart attacks, and a decreased chance of dying within 10 years.